Jovi CY Wong, MD, MSc, DPhil
University of Toronto
The American Society for Retina Specialists annual meeting in Stockholm, Sweden, kicked off with the Wet AMD Symposium I focusing mainly on gene therapies. This exciting opening session was moderated by Drs. Barbara Blodi and Donald D’Amico.
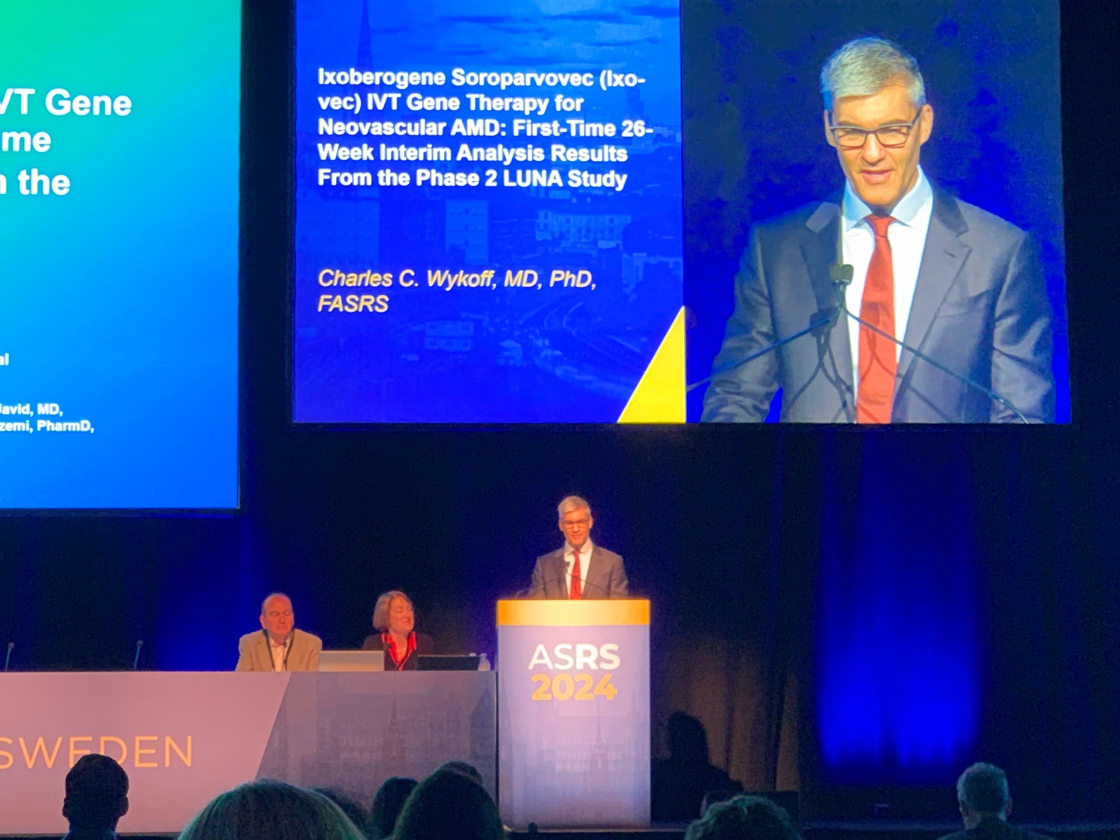
Dr. Charles Wykoff presented the latest results from the LUNA trial, for the first time including the 26-week interim analysis of Ixo-vec (Ixoberogene Soroparvovec) gene therapy for neovascular AMD. Ixo-vec is an intravitreal gene therapy that provides continuous intraocular aflibercept production. Because preliminary work with Ixo-vec had found significant intraocular inflammation, the LUNA trial was created to evaluate the efficacy of lower doses of Ixo-vec and 4 different corticosteroid prophylaxis regimens in previously treated patients with. Overall, 79% of patients remained injection-free at 26 weeks post Ixo-vec administration. No serious adverse effects were reported, however there was dose-dependent anterior chamber inflammation noted. The tested corticosteroid prophylaxis regimens were: difluprednate drops only, difluprednate with oral prednisone, difluprednate with intravitreal dexamethasone, and all three agents. Dr Wykoff reported that topical difluprednate was adequate in managing inflammation and that oral prednisone did not provide additional control, nor did the dexamethasone implant provide adequate control on its own. Further results will be reported in subsequent meetings as the LUNA trial is intended to continue for one year.
![]()
Following, Dr. Raj Maturi reported on the Phase 2 population extension cohort in the PRISM trial, which evaluates 4D-150, a dual transgene single dose intravitreal gene therapy for the treatment of nAMD. 45 patients were enrolled into two groups, a low and high dose of 4D-150. No serious adverse events were found. There was one report of vitritis in the high dose group. The regimen used included one dose of topical difluprednate with intravitreal aflibercept one week before 4D-150 administration, as well as aflibercept again 4 weeks after gene therapy to maintain control while gene expression is in progress. 77% of high dose patients and 60% of low dose patients were injection free at 6 months. 4D-150 is anticipated to enter Phase 3 in 2025.
![]() Next, Dr. Edward Wood then reported on the Phase 2 phamacodynamic study of the ABBV-RGX-314 anti-VEGF monoclonal antibody fragment subretinal gene therapy for nAMD. This gene therapy is being investigated in multiple trials for nAMD and diabetic retinopathy, as well as via both subretinal and suprachoroidal delivery routes. Dr. Wood reported specifically on the change in manufacturing process from an adherent hyperstack method which was smaller-scale and manual, to a suspension bioreactor process which is automated and scalable in anticipation of commercialization. The goal was to compare the clinical profile of 60 previously treated AMD patients treated with subretinal ABBV-RGX-314 who were randomized into four groups, low and high dose, and using the two different manufacturing processes. Dr Wood reported that subretinal ABBV-RGX-314 was well tolerated with no drug-related adverse events, and similar clinical profile between both manufacturing processes. 73% of patients were injection-free at 6 months in the bioreactor process compared to 80% from the hyperstack process.
Next, Dr. Edward Wood then reported on the Phase 2 phamacodynamic study of the ABBV-RGX-314 anti-VEGF monoclonal antibody fragment subretinal gene therapy for nAMD. This gene therapy is being investigated in multiple trials for nAMD and diabetic retinopathy, as well as via both subretinal and suprachoroidal delivery routes. Dr. Wood reported specifically on the change in manufacturing process from an adherent hyperstack method which was smaller-scale and manual, to a suspension bioreactor process which is automated and scalable in anticipation of commercialization. The goal was to compare the clinical profile of 60 previously treated AMD patients treated with subretinal ABBV-RGX-314 who were randomized into four groups, low and high dose, and using the two different manufacturing processes. Dr Wood reported that subretinal ABBV-RGX-314 was well tolerated with no drug-related adverse events, and similar clinical profile between both manufacturing processes. 73% of patients were injection-free at 6 months in the bioreactor process compared to 80% from the hyperstack process.
![]()
Lastly, Dr. Veeral Sheth presented on EYP-1901, a controlled release product containing vorolanib, which is a tyrosine kinase inhibitor, within durasert, a bio-erodible intravitreal insert. Dr Sheth presented data assessing supplemental injection use across groups in the Phase 2 DAVIO 2 trial of EYP-1901 vs aflibercept in wet AMD. Previously treated nAMD patients were randomized to low dose, high dose and q8week aflibercept. Previously, DAVIO 2 had shown that EYP-1901 maintained vision and CST, and had an acceptable safety profile, with no cases of severe adverse events. Dr Sheth proceeded to show that two-thirds of eyes were supplemental injection-free up to week 32. He also stated that the patients who required supplemental injections needed these based on prespecified criteria including BCVA reduction, CST increase, both, or vision-threatening hemorrhage. The reason for needing supplementary injections was most commonly due to both BCVA reduction and CST together but was fairly distributed amongst the prespecified criteria. 12% of low dose and 6% of high dose patients were given supplementary injections based on investigator discretion outside of the prespecified criteria. Dr Sheth also showed new 12 month data showed that vision change remained similar between EYP-1901 and aflibercept, with a planned upcoming Phase 3 trial.
The ensuing discussion included speculation on whether follow up for inflammatory sequelae of novel gene therapies could become somewhat burdensome especially considering that one major benefit of these therapies would include fewer visits needed. Another question related to delivery routes for these therapies which currently include subretinal, suprachoroidal, and intravitreal delivery, with discussion surround the benefits and drawbacks of these routes. These included the lower inflammatory burden but need for surgery in a subretinal injection, compared to higher inflammatory burden but perhaps greater efficacy and ease of administration for intravitreal routes of many of the tested therapies. The session closed with remarks that as a field, we are currently learning more about how gene therapies are tolerated in our patient populations as well as how best to manage any associated inflammation. Ultimately there will likely be room for various options from our tried-and-true regular anti-VEGF injections, to slow-release implants, to gene therapy, that we can use to address each of our patient’s needs.