Fiammetta Catania, MD, FEBO
Hospital Foundation Adolphe de Rothschild
The opening day of Floretina 2023 featured an intense and compelling X-Cases session moderated by Alexander J Brucker, Stanislao Rizzo, Bailey Freund, Anat Loewenstein, and Sandrine Zweifel.
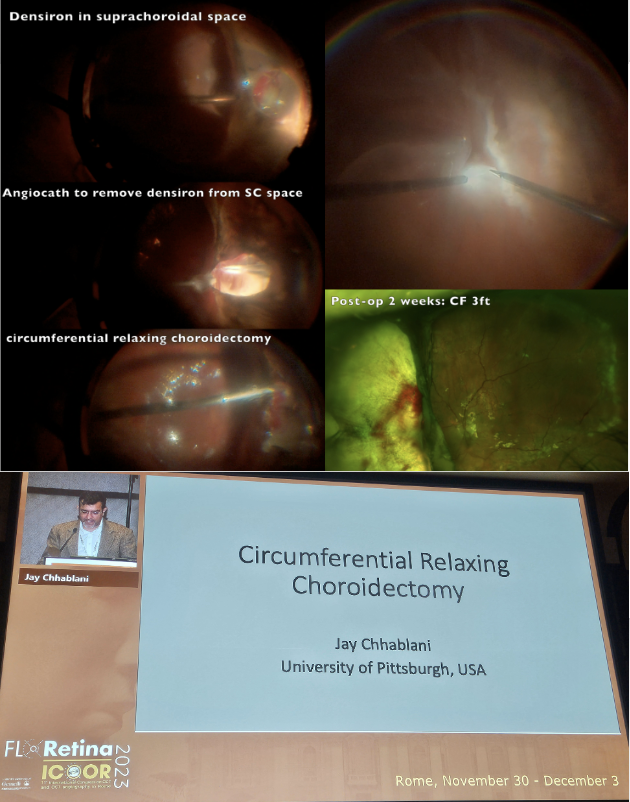
The session kicked off surgical cases, first up was Professor Jay Chhablani who presented a case of a 74-year-old female with a retinal detachment in the context of choroidal melanoma. The patient underwent pars plana vitrectomy, choroidal biopsy, membrane peeling, perfluorocarbon, silicone oil, and plaque radiotherapy. The patient subsequently developed a choroidal detachment with recurrent retinal detachment caused by the inadvertent prolapse of silicone oil into the suprachoroidal space. Prof Chhablani thus presented a surgical technique for removal of suprachoroidal silicone oil using an angiocath cannula followed by a circumferential choroidectomy, which allowed for a successful retina reattachment.
Next, Dr. David Chow described the case of a 65-year-old female with high myopia who developed a serous macular detachment in her better seeing eye. The detachment continued to expand to the posterior pole over the course of 1 year follow up, accompanied by a mild decrease in visual acuity from 20/40 to 20/50. The presence of peripapillary intrachoroidal cavitation (PP ICC) connected with the serous detachment was finally noticed. Slow but successful long-term reattachment was finally obtained after vitrectomy and ILM peeling with an innovative technique consisting of filling the cavitation with a graft of amniotic membrane. The case raises attention on PP ICC as a possible diagnosis in posterior pole serous detachments in highly myopic eyes. It can be recognized as an orange yellow lesion usually located inferiorly to a myopic disc.
![]()
Next, Dr. Ehab El Rayes presented an innovative technique for ab externo management of small recurrent retinal detachments in eyes that had previously undergone scleral buckling surgeries. He presented the case of a 32-year-old highly myopic (-12 D) male patient showing 2 small open tears located posterior to an inferior buckle placed for rhegmatogenous retinal detachment 7 months prior. The tears were out of reach of laser treatment. A suprachoroidal catheter was used to inject a Healon 5 bubble at the level of the retinal tears allowing indentation of the target retina and subsequent sealing of the tears with laser. Healon GV and Hyaluronic acid are also good alternatives to be used with the same procedure. The main difference between these agents is duration of the indentation: complete reabsorption of the substance occurs in 5-14 days for Healon 5, 45 days for Healon GV, and a few months for hyaluronic acid. No signs of toxicity were reported.
![]()
Not to be outdone, Dr. Oshima Yusuke presented the challenging surgical case of a 61-year-old female with a history of radial keratotomy as well as a chronic retinal detachment with PVR and dense cataract in the context of a myopic macular hole. Preoperative vision was CF. In this case peeling of the PVR and ILM under perfluorocarbon helped release traction and lead to macular hole closure. He used C3F8 as a tamponade and IOL implantation was postponed for a second surgery 2 months later. The final VA post cataract surgery was 20/200.
![]()
The next session of cases focused on maintaining a differential diagnosis while evaluating patients. First up was Professor Bertil Damato who presented a case of a fast growing apparently benign choroidal nevi. The patient was a 73-year-old female with an inferonasal choroidal nwevus with no red flags for melanoma suspicion except for a tumor growth rate per year of 21.7% documented during 4 years of follow up. Considering that normal growth rate for a choroidal nevus is 1% per year and for choroidal melanomas, the grow rate is roughly 30% per year, the patient was treated with transpupillary thermotherapy. The take home message is to pay attention to fast enlarging choroidal nevi especially in elderly patients and to not underestimate lesions with a zero MOLES score.
![]()
Next, Dr. José Garcìa-Arumì discussed the case of a 47-year-old patient who was referred for loss of vision in the left eye. Symptoms started 1 year before and the vision at the time of referral was now hand motion. On exam, there was a 360° choroidal detachment, exudative retinal detachment, and a posterior tumor concerning for a choroidal melanoma. Ultrasound revealed a posterior dome shape tumor with a basal diameter of 14.28 mm and a 5.80 mm thickness. In the nasal portion of the tumor, there was concern for an extrascleral nodule. OCT reveled irregularity of the tumor surface and marked hyperreflectance of the RPE/Bruch membrane complex. A PET CT scan, pars plana vitrectomy (PPV) transvitreal biopsy, cytogenetics and immunohistochemistry was proposed. The patient refused and came back 5 months later showing a progression of the extrascleral lesion, increased tumor size, and conjunctival hyperemia and chemosis. At this time, PET CT scan revealed an orbital hyperactive mass with submandibular lymphadenopathy. Orbital biopsy showed a friable gelatinous mass with positive immunohistochemical B phenotype marker for neoplastic cells. The diagnosis of MALT choroidal lymphoma was made and the patient was subsequently treated with external radiotherapy. Despite the atypical presentation (young age, simultaneous intraocular and orbital involvement), some typical signs oriented the diagnosis, notably the irregularity of the choroid and the hypereflectivity of the RPE/Bruch complex.
![]()
The next case was by Dr. Joussen Antonia who discussed the rare differential diagnosis of “Dark lesions” of the ocular fundus. In the first case a 58-year-old patient was referred for subacute vision loss and multiple dark lesions in the left eye. On further history it was noted the patient had undergone previous excision of a cutaneous melanoma two years prior. A diagnosis of metastasis of cutaneous melanoma was posed. In the second case, a 58-year-old patient with a presumed diagnosis of choroidal melanoma was sent for a second opinion. In this patient, the choroidal lesion disappeared with upgaze and reappeared with downgaze. A diagnosis of a congested vortex vein was made. The third case was that of a 54-year-old female with blurred vision and fatigue. Exam in this patient revealed multiple bilateral dark lesions compatible with the diagnosis of bilateral diffuse uveal melanocytic proliferations (BDUMP). This is a rare paraneoplastic syndrome that prompted Dr Joussen to ask for a upper endoscopy in search of a primary tumor. The procedure revealed the presence of a moderately differentiated adenocarcinoma of the stomach (intestinal type).
![]()
Next, Dr. Marion Munk presented a case of a 57-year-old Caucasian male experiencing vitreous floaters in his right eye along with shortness of breath. The patient had a negative CT chest and bronchoalveolar lavage. Diagnostic workup revealed a IL10/IL6 ratio of 2, a protein electrophoresis suggestive of monoclonal gammapathy, and extensive histiocytosis without granulomas at lymph node biopsy. PET and MRI scans were negative as well. ACE and MYD88 levels were normal. FA revealed disc leakage, areas of non-perfusion, and no granulomas. Suspecting sarcoidosis, the patient was prescribed oral corticosteroids without therapeutic success. The patient also underwent vitrectomy but the floaters recurred 2 months after surgery. Further history revealed, that a family member also had similar signs and symptoms. Thus, biopsy of the abdominal fat was performed and revealed congophil accumulations with apple green birefringence, diagnostic of amyloidosis. Genetic testing helped pose the final diagnosis of familial ATTR Amyloidosis.
![]()
Next, Dr. Ramin Tadayoni presented the case of a 63-year-old hyperopic patient with a history of peripheral iridotomy and mild vision loss. Multimodal imaging showed macular foveoschisis at the level of the Henle fiber layer without evidence of epiretinal membrane or optic pit. A diagnosis of stellate nonhereditary idiopathic foveomacular retinoschisis was eventually made in this patient.
![]()
Next up, Professor José Maria Ruiz Moreno presented the case of a 63-year-old female with a stage 2 macular hole in her left eye. Following surgical repair, the patient developed macular atrophy with diffuse outer retinal and RPE damage. Prior to her surgery, she had received paclitaxel, pertuzumab, and trastuzumab for breast cancer. The treatment with paclitaxel had been interrupted 19 months before the vitrectomy. The unifying diagnosis explaining the postoperative findings was photosensitivity to endolaser induced by treatment with paclitaxel. The particularity of this case is that photosensitization normally ends within a few weeks from treatment interruption while this case raises the suspect of a possible long-term storage of the drug in retinal tissue in some patients.
![]()
Lastly, Dr. Gaurav Shah reported the case of a 49-year-old patient with sudden bilateral vision loss due to multiple serous retinal detachments. The patient was affected by stage 4 lung cancer and was treated with pembrolizumab and solumedrol. The interruption of treatment with pembrolizumab resulted in the complete resolution of the retinal lesions in 2 weeks, which led to the diagnosis of pembrolizumab induced Vogt Koyanagi Harada syndrome. Pembrolizumab is a programed cell death 1 inhibitor (PD-1) used to treat melanoma, lung cancer, head and neck cancers, Hodgkin lymphoma, stomach cancer, cervical cancer, and certain types of breast cancers. Genetic predisposition for VKH has been reported in patients with HLA-DR4/DRB1*04 haplotypes. CTLA-4 and PD-1 genetic polymorphisms have been found in VKH patients previously. These molecules are checkpoints related to immune tolerance and these polymorphisms can be associated with a break in immune tolerance. Attention should be paid to the fact that delayed intolerance to anti-PD-1 agents up to 16 months after the last dose of the drug has been reported in literature.
![]()
The session displayed interesting and varied cases, spanning from drug toxicity to innovative surgical techniques. Many presenters pointed out the importance of paying attention to details and to not underestimate common ocular symptoms which may be masquerading more sinister diagnoses.