Emanuele Crincoli, MD, FEBO
Policlinico Universitario Agostino Gemelli
An advanced instructional course on the impact of digital innovations on retinal care was held in Floretina 2023 meeting in Rome. The course organized by Anat Lowenstein, Joel Hanhart and Adnan Tufail was aimed at exploring beneficial and detrimental aspects of digital innovations in real life management of retinal diseases. Both technical and socioeconomic aspects of the topic were discussed.
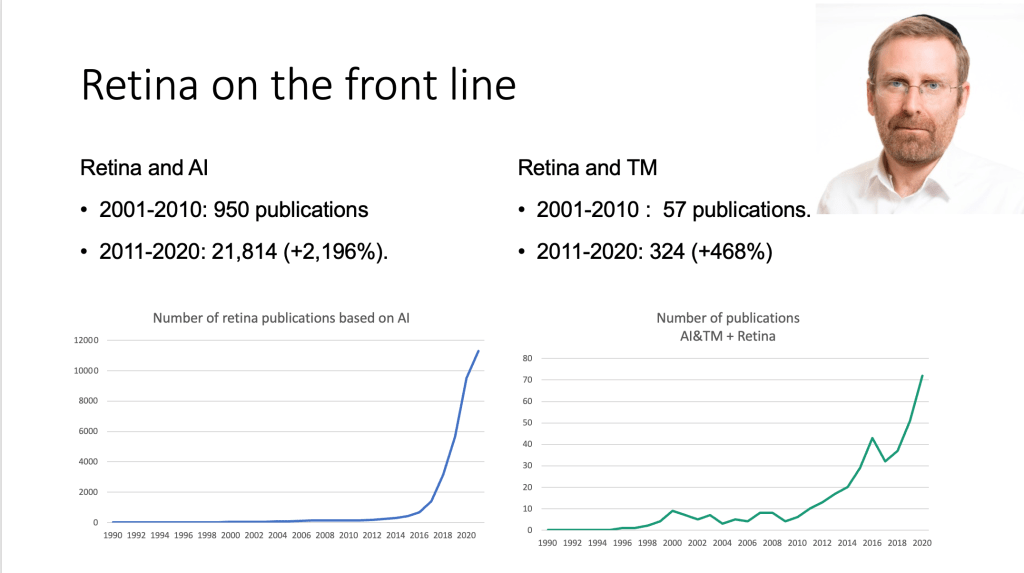
The course was introduced by the presentation “Redefining the medical encounter: towards an anthropologic shift” by Dr. Joel Hanhart (University of Jerusalem) (above). This talk focused on how telemedicine (TM) and artificial intelligence (AI) are revolutionizing the doctor-patient relationship and gaining an increasingly prominent role also due to geopolitical contingencies such as war and the COVID-19 pandemic. TM and AI also gained increasing attention in ophthalmology research in the last decade, with 34552 articles produced from 2010 to the present date compared to the approximately 2000 produced in all prior decades combined. Dr. Hanhart then analyzed anthropological, philosophical and spatial consequences of these innovations, concluding that AI will force us to reshape clinical practice in order to preserve the core of doctor-patient relationship.
![]()
In the second talk, Dr. Tunde Peto (Queen’s University Belfast) (above) explored “The boundaries of telemedicine.” The presentation highlighted the importance of imaging in TM and gave an overview of hand-held ultraportable retinal imaging devices available on the market, allowing 5–60-degree fields of view imaging for TM purposes. Most of these technologies still require validation in larger studies, even though some real-life experiences such as the REACH RD project in the Philippines are showing promising results. Concerning pitfalls of TM in diabetic retinopathy (DR) care, Dr. Peto highlighted how wider field imaging would be required for accurate evaluation and how AI shows good performance in detecting “existing” elements (i.e. intraretinal fluid) but struggles to detect “missing” elements (i.e. atrophy).
![]()
Most of the course was dedicated to more technical aspects. Dr. Emanuele Crincoli (Agostino Gemelli University Policlinic) (above) gave an intense overview of the “Use of AI in screening and diagnosis of retinal conditions.” After a quick introduction on the different demands for healthcare assistance in various settings in the modern society, Dr Crincoli focused on real-life applications of existing technologies in the management of common retinal diseases.
Regarding DR, he described the improvement in diagnostic accuracy brought by the advent of deep learning (DL) technology, stressing the importance of the specificity of screening methods. He also presented various software for automatic DR detection and staging, focusing on EyeArt software (EyeNuk Inc.). This recently FDA approved software allows accurate detection of more than moderate DR (96% sensitivity, 88% specificity) and vision threatening DR (97% sensitivity, 90% specificity). Sensitivity of this screening method was proven to be significantly higher than dilated fundus inspection by both retina specialists and general ophthalmologists (60% and 21%, respectively).
Regarding age-related macular degeneration (AMD), he presented the results of the FDA-approved iPredict AMD software in detection of referrable AMD on color fundus photographs (CFP). The same software also provides a personalized assessment of the risk of advanced stage AMD development withing 1 and 2 years. CFP also allows accurate diagnosis and staging of myopic maculopathy, with good performances in the detection of lacquer cracks, myopic neovascularization and Fuchs spots. For tractional complications, OCT based DL models might be preferred instead. The use of soft labeling might represent a turning point in the improvement of models aimed at classification of diseases with poor imageability.
Besides the applicability for screening purposes, Dr. Crincoli also explored innovative and more advanced applications of AI in retinal diseases, which might support tertiary care management and research in the future. These models, based mainly on microscopic imaging techniques such as OCT, can help predict natural history of a condition (such as time to exudation of non-exudative macular neovascularization) and response to treatment (such as in the case of subretinal and intraretinal fluid monitoring). They may also help in the identification of new biomarkers that can improve diagnostic performance of human graders and improve understanding of the pathologic mechanisms of a disease. The closing segment was dedicated to AI pitfalls, with a focus on the issues coming with big data management (i.e. adversarial attacks, privacy) as well as legal and economic issues associated with the trustworthiness of AI.
![]()
In the fourth presentation (“New biomarkers for the evaluation of AMD: Booms and Busts”), Dr. David Sarraf (UCLA Stein Eye Institute) (above) illustrated the impact of OCT and OCTA on AMD management and concentrated on the future applications of these technologies. In particular he focused on 3 interesting areas of application of AI: non-exudative AMD, subretinal hyperreflective material (SHRM) and fluid quantification.
![]()
In the last presentation of the session entitled, “The example of Discovery, an AI-developed program. Is the patient still in the center?” Dr. Lorenzo Ferro Desideri (Inselspital University Hospital Bern) (above) discussed the potential clinical applications and possible pitfalls in the adoption of Discovery, a novel AI-derived platform. This platform provides automatic segmentation and measurement of retinal thicknesses, volumes and biomarker detection, allowing clinicians to better understand and describe OCT biomarkers associated with different retinal diseases. A recent study published in Retina1 by the author analyzed the role of Discovery in the prediction of the clinical course of central serous chorioretinopathy (CSCR). The AI-derived platform allowed the differentiation of acute CSCR from chronic CSCR, by describing the presence of thicker outer nuclear layers and higher amount of subretinal fluid in the first group. Moreover, Dr. Ferro Desideri showed the application of this software in other retinal diseases, including white dot syndromes, diabetic retinopathy, and rhegmatogenous retinal detachment (RRD), in which preliminary data reported the presence of novel biomarkers (like hyperreflective foci) predictive for worse visual outcomes in patients operated on for macula-off RRD.
In the second part of the presentation, the limitations and pitfalls related to the use of this AI platform were discussed, including the presence of technical errors in the automatic segmentation, the need of continuous updates and revisions of the current clinical classifications in order to improve AI analysis, and the ethical aspects of using AI in ophthalmology. In conclusion, Dr. Ferro Desideri pointed out promising results in the adoption of this AI-derived platform in the diagnostic and prognostic framework in patients with retinal diseases; however, we should never forget about the human patient and the larger clinical picture.
The session provided an excellent overview of the recent updates in AI and retina while facing important issues that need to be resolved for this revolution to take place in the safest and most effective way.