Chloe Y. Li, MD
Columbia University/New York Presbyterian, New York City, NY
Clinical trial results dominated this year’s Late-Breaking Abstracts session at Retina Subspecialty Day, featuring new results from trials testing already-approved therapies as well as results from therapies in early clinical trials.
Discussing treatments for diabetic macular edema and geographic atrophy respectively, Dr. Diana Do and Dr. Dilsher Dhoot revealed results from extension studies of high dose aflibercept and pegcetacoplan. Dr. Do presented results from the PHOTON extension study, which established the non-inferiority of 8mg aflibercept every 12 or 16 weeks, as compared to 2mg aflibercept every 8 weeks, in the treatment of diabetic macular edema (DME). 70 patients who had been dosed with aflibercept 2mg every 8 weeks during the original PHOTON study crossed over to 8mg every 12 weeks, while 195 patients were continued on 8mg every 12 weeks or 16 weeks. Patients were followed for an additional 60 weeks after the conclusion of PHOTON. All patients maintained a 7.7 letter improvement in vision and mean 187.9 micron decrease in central retinal thickness (CRT) throughout the 60-week study period. Patients who crossed over from the 2mg every 8-week group achieved less variability in their CRT and vision on higher doses of aflibercept, and 83% of patients of them could be dosed at greater than 12-week intervals at the last study timepoint.
Dr. Dhoot presented extension data from the OAKS, DERBY, and GALE studies, which investigated the effect of pegcetacoplan on subfoveal geographic atrophy (GA). Most patients (65%) in the OAKS and DERBY studies had subfoveal GA, which enlarges at a slower rate than GA elsewhere in the macula. Dr. Dhoot argued that despite this slower growth rate, subfoveal GA is important to treat because 82% of patients in OAKS and DERBY with subfoveal GA still had better than 20/200 vision, and therefore have significant vision to lose. In the GALE study, patients who had been on pegcetacoplan in OAKS and DERBY continued the drug, while patients who had been on sham injections were crossed over to either pegcetacoplan monthly or every other month. Patients were followed for 36 months. Because all patients were receiving pegcetacoplan by the end of the study, a projected sham growth rate of GA was extrapolated from the first 24 months of the study, during which a real sham group existed. By the end of year 3, the monthly dosing group had 31% less enlargement in subfoveal GA lesion and the every-other-month group had 25% less enlargement as compared to sham. However, at the end of year 1, this difference was almost indiscernible. Similarly, when treated eyes with GA were compared to fellow eyes with GA, at the end of year 3 monthly pegcetacoplan eyes had a 29% reduced rate in GA lesion growth and every-other-month eyes had a 24% reduced rate of GA growth. Functional results showed that at months 24 and 36, eyes treated with monthly pegcetacoplan had significantly fewer scotomas on microperimetry than eyes; however, eyes treated with every-other-month pegcetacoplan did not differ in microperimetry testing from sham at any time point. At the last study timepoint, zero new cases of retinal vasculitis were reported, and Dr. Dhoot suggested that its development is a first-injection phenomenon following pegcetacoplan treatment.
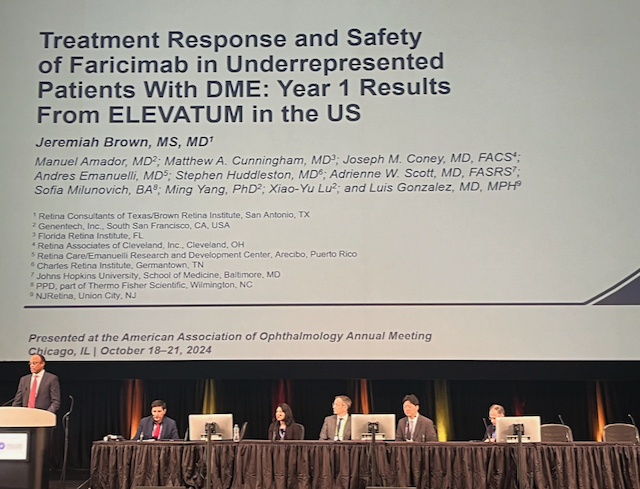
Dr. Jeremiah Brown presented results from ELEVATUM, which aimed to test the safety and efficacy of faricimab for treating DME in underrepresented patient populations. 154 treatment-naive patients with A1c less than 12 were enrolled, with 45% Hispanic, 45% African American, and 10% Native American and Pacific Islander patients. Patients received 6mg faricimab every 8 weeks, the same dosing protocol as used in the YOSEMITE and RHINE studies. Hispanic patients in ELEVATUM had significantly worse vision and DME and severity of diabetic retinopathy (DR) on initial enrolment as compared to African-American patients. Patients of all races and ethnicities had improved vision and DME after treatment with faricimab. Hispanic patients had the greatest improvement in vision and severity of DME and DR, possible because they had the most severe disease at enrollment. The safety profile of faricimab was similar in ELEVATUM as in YOSEMITE/RHINE, with zero cases of endophthalmitis. Panelists during the discussion pointed out that patients have much diversity that cannot be captured with categories of race alone, and that the many social determinants of health cannot be captured with these categories.
Drs Joel Pearlman and Alex Melamud presented on novel systemic therapies for retinal diseases, with Dr. Pearlman showing the effect of the kallikrein inhibitor RZ402-201 on DME, and Dr. Melamud the effect of gildeuretinol on geographic atrophy.
![]()
In testing RZ402-201, Dr. Pearlman and collaborators administered different doses of the drug (50, 200, and 400mg) as well as placebo to groups of 25 patients with mild to moderate NPDR and DME. No patients had more than 3 anti-VEGF injections, and none within 8 weeks of study initiation. The drug was tolerated well at all doses, with few mild adverse events such as hypertension or gastrointestinal side effects; no severe AEs were reported. Patients on 50mg and 200mg daily of the drug had significantly improved central subthreshold thickness on OCT by week 12, the end of the study period. Patients on the 50mg and 200mg doses had slight but significant increases in vision, though the placebo patients also did. Dr. Pearlman argued that the 400mg dose group did not have improved CST due to complete saturation of plasma kallikrein. The drug is thought to inhibit endothelial kallikrein, thus inhibiting downstream vascular permeability and injury. When asked why RZ402-201 could not be delivered intravitreally, Dr. Pearlman answered that intravascular and endothelial inhibition of kallikrein could not be achieved as well with an intravitreal drug as with an oral drug. Given its safety and efficacy in decreasing CST, this drug offers a potential augmentation option for anti-VEGF treatment.
![]()
Dr. Melamud and collaborators presented the effect of gildeuretinol, vitamin A which is modified with heavy hydrogen, on GA in dry AMD and Stargardt’s disease. These two diseases are driven by the accumulation of lipofuscin, a metabolic waste product of the visual cycle produced following the dimerization of vitamin A. Because gildeuretinol slows vitamin A dimerization, Dr. Melamud tested whether it could slow the progression of geographic atrophy. 135 patients with GA were given daily oral gildeuretinol, while 63 were given a placebo drug. The rate of adverse events and withdrawal from study was comparable between placebo and study groups. No intraocular inflammation, vasculitis, or signs of hypervitaminosis or hypovitaminosis A were attributed to the drug. The investigators planned to perform sensitivity analysis after 6 months of drug administration, given the amount of time estimated to replace systemic vitamin A stores in patients. Analysis of GA area and low-luminance visual acuity between patients on gildeuretinol and placebo showed significantly decreased GA lesion growth rate and preserved vision at 24 months. Gildeuretinol is the first oral drug to show functional benefit in geographic atrophy.
Finally, Dr. Eric Schneider presented results on the use of home OCT to quantify disease severity and progression in neovascular AMD, as well as the ability of an AI program to identify these biomarkers in home OCT. First, expert graders compared home OCT images to in-office OCT images. Patients took at home OCT images daily for 5 weeks, and had in-office OCT at the initial enrollment visit, at Week 1, and Week 5. Total retinal hyporeflective space (representative of subretinal or intraretinal fluid) was used as the comparative biomarker between home and in-office OCT. 180 patients with neovascular AMD in one eye were enrolled. 96% of patients were able to comply with daily OCTs, and the positive agreement rate between home and in-office OCT on presence of TRO was 86%, whereas the negative agreement rate on absence of TRO was 87%. Then, an AI algorithm was used to test the similarity of TRO on home OCT images versus in-office OCT images. 336 patients with neovasacular AMD in one eye were enrolled, and each received OCT imaging on two machines on home and OCT imaging on one machine in the office. AI reading of home OCT images were compared to human expert grading of office OCT images. The coefficient of variation for volume of TRO in the AI-graded home OCT images was 11.1%, compared to 16.4% for the human-graded office images, suggesting that the AI-graded home OCT images were reliably repeatable and could be used to identify TRO at home. There was a high degree of fidelity between AI-graded and expert-graded agreement, as the DICE score was similar between AI compared to experts versus experts compared to experts.